By Marina Matsiukhova
Guest Post: Nursing Theory In The Real World: 4 Ways To Apply Orem’s Theory of Self Care to Your Daily Practice
Mar 1, 2017 1:55:00 PM / by user posted in nursing theory, guest post
Guest Post: The Expanding Opportunity for Advanced Practice Clinicians
Dec 20, 2016 2:13:00 PM / by user posted in advanced practice, Nurse Practitioner, guest post
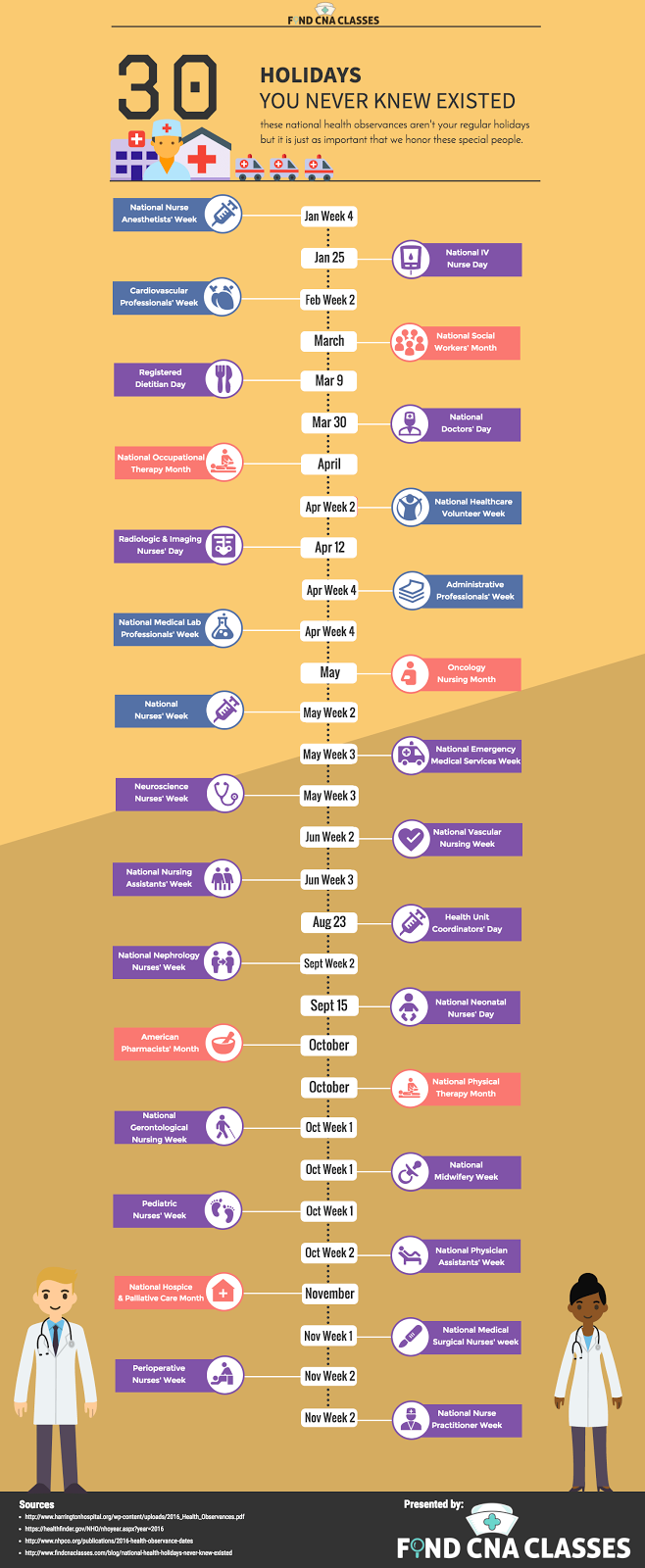
Holidays for Healthcare Professionals
Nov 16, 2016 4:13:00 PM / by user posted in nursing, guest post, infographic
Top 7 Long Term Benefits of Certified Nursing Assistant Programs
Oct 31, 2016 11:51:00 AM / by user posted in CNA, guest post
A better solution to Prior Authorization with medications
Jul 20, 2016 12:08:00 PM / by user posted in Nurse Practitioner, nursing, guest post, medication administration
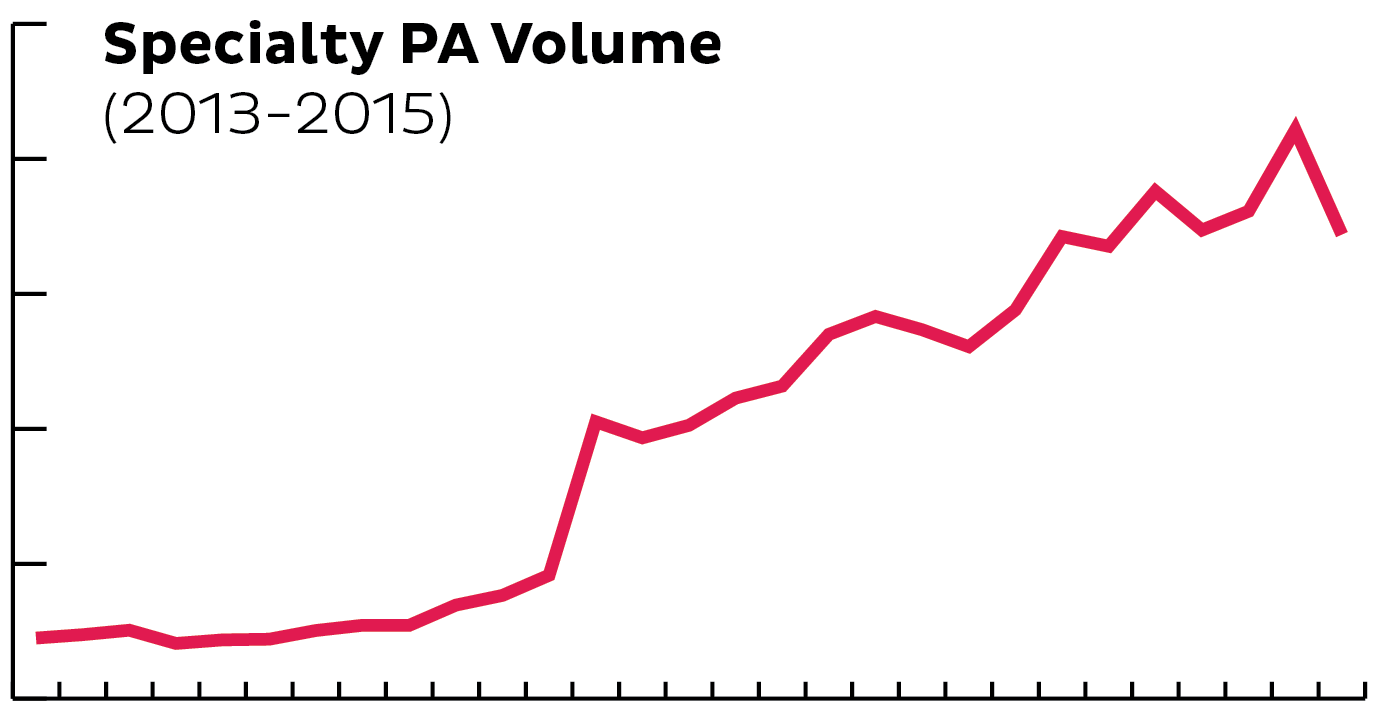
Nurses: With Specialty Meds on the Rise, You Need a Better PA Solution
Specialty medications often manage chronic disorders (multiple sclerosis, hepatitis C and immune deficiencies are a few examples), and can require special administration (i.e., through injectable or intravenous (IV) infusion).
So is PA required for all specialty medications?
While there are always exceptions, specialty medications likely require a PA request. With a significant increase in specialty meds, we’ve seen a direct correlation to PA requests spiking as well. As new medication continues to develop, this will be something that continues to trend upward.
What takes the PA process so long, anyway?
First, let’s review a quick definition:
- Prior Authorization: The patient’s prescription coverage plan needs extra information about why your patient needs the prescribed medication in order to determine benefit coverage.
The PA process involves several parties (pharmacy, doctor, health plan, patient) and is often time consuming. CoverMyMeds steps in to limit the inevitable back and forth, with an electronic, streamlined solution for nurses and their staff. Instead of printing a form, manually filling it out and sending a paper copy to the plan, you can now complete all requests, from start to finish, through the CoverMyMeds web portal or directly through your electronic health record (EHR), at no cost.
Wait, so who are you again?
Our story began back in 2008 when a pharmacist and a tech guy questioned, “Why won’t the health plan just cover my meds?” Today, we are the leading electronic prior authorization (ePA) company in the nation, helping more patients receive the medications they need in order to live healthier lives. In fact, more than 600,0000 providers and staff use CoverMyMeds to manage PA requests, along with 80 percent of the pharmacy network, nationwide.
As a Provider or Medical Professional, how do I make the process easier, like you mentioned? An electronic solution, such as CoverMyMeds, is your best bet. You may already have access to manage PA requests within your EHR system. If not, it’s easy to get started with the CoverMyMeds HIPAA-compliant online portal. Simply create a free account or log in to complete your next PA request in minutes!
By completing PA requests electronically, your office will save time, reduce administrative waste and help patients get the medications originally prescribed. On average, users indicate they complete PA requests in 3-5 minutes through CoverMyMeds versus the traditional fax or phone process, which often requires 15-20 minutes. The CoverMyMeds solution works with all health plans and for any drug (retail and specialty). This is important to ensure you only need to work through one process for any scenario — even Medicare and Medicaid.
Want personal help getting started?
Live chat our PA experts or call 1-866-452-5017.